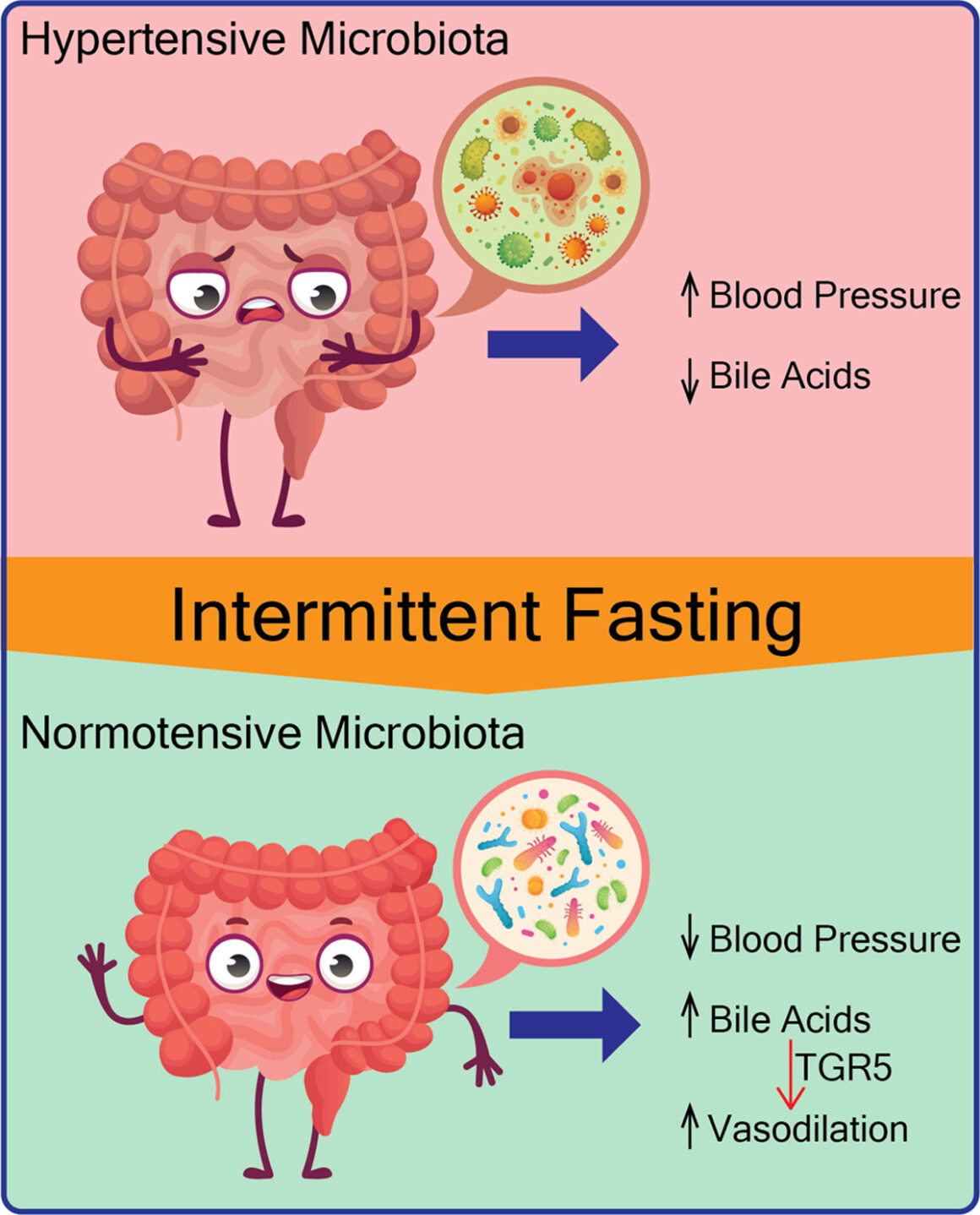
Previous studies have shown that a harmful combination of gut bacteria can cause high blood pressure (hypertension) in humans and other animals. Having a harmful combination of bacteria in the gut is called gut dysbiosis. There aren’t any well-established methods or drugs that reliably change the bacteria make-up in the gut to treat gut dysbiosis. A new study recently showed that when rats with high blood pressure caused by a gut dysbiosis were placed on an intermittent fasting eating schedule, the bacteria make-up in the rats’ intestines changed and the high blood pressure went away. This suggests that an intermittent fasting schedule might permanently correct high blood pressure in a person who has it due to gut dysbiosis.
Which Intermittent Fasting Schedule Was Used?
The rats in the study’s intermittent fasting group were fed on an every-other-day (EOD) “ad lib” schedule. This means that for 24 hours, they could eat as much as they wanted, whenever they wanted. For the next 24 hours, the rats had access to water but not food, and then this cycle was repeated. Even though the rats on the EOD schedule had unlimited access to food on their eating days, they didn’t catch up on their eating days. They ate about a third less total food than the rats with all-day, every-day access to food.
How Long Did the BP Change Take?
After two weeks on the every-other-day IF schedule, rats with problem-causing gut bacteria had significantly lower blood pressure than the rats with the same problem-causing bacteria that were eating as they pleased (an every-day, all day ad lib diet). The beneficial effect lasted for the duration of the study (10 weeks).
Was the Improvement Permanent?
The researchers didn’t look to see whether the rats with improved blood pressure maintained it when they resumed an every-day, all-day ad lib diet.
Was the Problem Transferable?
After the two-week feeding experiment, the researchers tested a third population of rats: rats that had sterile guts (no bacteria in their guts). The researchers separated the sterile-gut rats into two groups. They transferred bacteria from the IF rats into one group and bacteria from the ad lib feeding rats into a second group. The rats is both sterile-gut rat groups had normal blood pressure before the bacterial transfer.
After the transfer of bacteria, the rats that received bacteria from the ad lib group developed significantly higher blood pressure than those receiving bacteria from the IF group.
What Does This Mean?
For people who have high blood pressure, an intermittent fasting (IF) schedule may be beneficial. A person can easily self-check blood pressure, so testing blood pressure changes before and then after adopting an IF eating schedule is something a person can safely add to their “study of one.” Rats don’t live as long as humans, so changes in humans that are similar to the rats in this study may take longer. A shorter fasting interval, such as Fast-5’s 19/5 cycle, may take longer to work than the study’s 24/24 every-other-day cycle.
Bacteria Don’t Know What Time It Is, So How Could an Intermittent Fasting Schedule Change Gut Bacteria?
Bacteria living in the gut influence what is absorbed from the gut. The researchers conducting this study looked at several metabolites (chemicals made or altered by bacteria) to see which ones might be involved. They found that bile acids, which are chemicals secreted by the liver and reabsorbed downstream in the gut, were more likely than others to be key factors in the changes they saw. Because bile acids are reabsorbed by the gut, they wind up in the bloodstream where they could have an effect on blood pressure through another chemical called TGR5.
However, after transplanting the bacteria from rats with high blood pressure to sterile-gut rats, researchers didn’t see the changes in bile acids in the recipient group, even though the rats in that group developed high blood pressure. That suggests that the changes in bile acids may be related, but aren’t a complete explanation for the blood pressure changes seen in the rats.
What If I’m Taking Medicine for High Blood Pressure?
If you’re taking medicine for high blood pressure, talk to the prescribing doctor about trying intermittent fasting for several weeks in a study of one. Because blood pressure is relatively easy and inexpensive to measure frequently, it should be easy to monitor safely. If there is a consistent improvement, it is likely going to be obvious. You can check and record your blood pressure yourself and give the records to your doctor to review. If an intermittent fasting schedule decreases or normalizes your blood pressure, you may be able to reduce or stop taking your blood pressure medicine. Do so only under the guidance of your prescribing doctor.
Is There Conflicting Evidence?
There is some conflicting evidence from other studies and from direct experience with Fast-5. Not everyone with high blood pressure who has started Fast-5 have seen it resolve, but some have. Some studies on humans reported seeing blood pressure increase on a fasting schedule, and others have seen decreases. For example, in one 8-week study, researchers compared subjects who ate one-meal-per-day with subjects who ate three meals per day. The researchers reported an unexplained drop in blood pressure for the 3-meal-per-day subjects, while the one-meal-per-day group had a slight increase in their average BP. The authors offer that this may have been due to the fact that the BP was measured in the morning among the 3-meal-per-day group and in the late afternoon for the one-meal-per-day group.